Bipolar vs. Schizophrenia: Understanding Differences & Taking a Schizophrenia Test
Feeling confused by mental health symptoms that might suggest either bipolar disorder or schizophrenia? You are not alone. Many serious conditions share overlapping signs, making self-assessment difficult and often misleading. If you find yourself searching for a bipolar or schizophrenia test, it’s a sign that you are seeking clarity, which is a courageous first step. Understanding the nuances between these conditions and considering a preliminary schizophrenia test can be very helpful. Do I have schizophrenia test? This is a question that deserves a careful and compassionate exploration. This guide will clarify the key distinctions between bipolar disorder and schizophrenia, helping you understand their unique features and why professional insight is crucial for your well-being.
Navigating these concerns can feel isolating, but understanding the landscape is empowering. While this article provides information, a preliminary self-assessment can help organize your thoughts. You can use our confidential symptom assessment by using a confidential tool designed to screen for early symptoms.
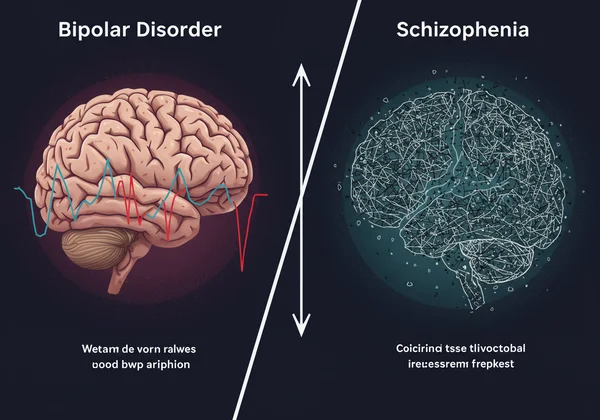
Schizophrenia vs. Bipolar Disorder: Core Symptom Differences
At a glance, schizophrenia and bipolar disorder can seem similar because both can involve psychosis. However, their core features and the patterns they follow are fundamentally different. Understanding these differences is the first step toward getting the right kind of support. The primary distinction lies in whether the symptoms are rooted in mood or thought processes.
Understanding Psychotic Symptoms: Hallucinations and Delusions
Psychosis is a state where a person's thoughts and perceptions are disrupted, making it difficult to recognize what is real. Both conditions can feature psychotic symptoms like hallucinations (seeing or hearing things that aren't there) and delusions (strong, false beliefs). In schizophrenia, these symptoms are a defining, persistent feature of the illness. They can occur at any time, independent of the person's mood.
In bipolar disorder, psychosis is typically linked to severe mood episodes. For example, a person in a manic state might have grandiose delusions, such as believing they have superpowers. Conversely, during a severe depressive episode, they might experience delusions of guilt or worthlessness. The key difference is that when the mood episode subsides, the psychotic symptoms often do as well.
Distinguishing Mood Episodes from Disorganized Thinking
Bipolar disorder is primarily a mood disorder characterized by extreme shifts in energy, mood, and activity levels. These shifts manifest as manic episodes (high energy, euphoria, irritability) and depressive episodes (low energy, sadness, hopelessness). While thinking can be affected during these episodes, the core issue is the dysregulation of mood.
Schizophrenia, on the other hand, is primarily a thought disorder. Its hallmark symptoms include disorganized thinking, difficulty concentrating, and "negative" symptoms like social withdrawal, lack of motivation (avolition), and a flat emotional affect. While mood disturbances can occur in schizophrenia, they are not the central feature as they are in bipolar disorder. A free schizophrenia test can help screen for these specific thought-related experiences.
The Role of Differential Diagnosis in Mental Health
Because of the symptom overlap, clinicians perform a differential diagnosis in mental health to distinguish between conditions. This isn't a quick checklist; it's a comprehensive process of gathering information to arrive at the most accurate conclusion. This process ensures that the treatment plan precisely targets the underlying condition, which is critical for a positive outcome.
A professional will look beyond the immediate symptoms to understand the bigger picture of your experiences. This includes your personal history, family history of mental illness, and how your symptoms have evolved. They will systematically rule out other medical or psychiatric conditions that could be causing your symptoms before settling on a diagnosis.
Examining Symptom Duration, Severity, and Impact
A key part of differential diagnosis involves examining symptom duration and its impact on your life. For a bipolar I diagnosis, a person must have experienced at least one full manic episode. For schizophrenia, symptoms like delusions, hallucinations, or disorganized speech must be present for a significant portion of time during a one-month period, with continuous signs of the disturbance persisting for at least six months.
The timeline is crucial. A clinician will ask: when did the symptoms start? Do they come and go, or are they constant? Are psychotic symptoms only present during mood swings? Answering these questions helps build a clear timeline that can point more definitively toward one diagnosis over the other. Taking a preliminary schizophrenia assessment test can provide a structured way to recall these experiences over the past month.
How Professionals Distinguish Mood Disorders from Psychosis
The core task for a professional is to distinguish mood disorders from psychosis as a primary issue. They will carefully assess the relationship between mood episodes and psychotic symptoms. If psychosis occurs exclusively during periods of mania or depression, a diagnosis of bipolar disorder with psychotic features is more likely.
If psychotic symptoms persist for two or more weeks in the absence of a major mood episode (manic or depressive), schizophrenia is more likely to be considered. Schizoaffective disorder is another possibility, where symptoms of both schizophrenia and a mood disorder (like bipolar disorder or depression) are present. This complexity underscores why self-diagnosis is unreliable and professional evaluation is essential.
Why Professional Assessment is Crucial for an Accurate Diagnosis
While online searches and preliminary tests are useful starting points, they can never replace a professional assessment. A trained psychiatrist or psychologist uses their expertise to interpret the subtle nuances of your symptoms in the context of your entire life. Taking an online schizophrenia test can help you prepare for this, but a professional provides a safe, non-judgmental space to explore your concerns and create a tailored treatment plan.

An accurate diagnosis is the foundation of effective treatment. The medications and therapies for bipolar disorder and schizophrenia are very different. The wrong diagnosis can lead to ineffective treatment, unnecessary side effects, and prolonged suffering. Trusting a professional with this process is an investment in your long-term health and recovery.
Preparing for Your First Mental Health Consultation
Feeling anxious about your first appointment is completely normal. Preparing for your first mental health consultation can make the process feel less daunting. Before you go, consider jotting down a few notes about your symptoms, when they started, and how they affect your daily life. Think about any major life events that occurred around the same time.
Using an online tool like the one on our homepage can help you organize these thoughts. You can start your online assessment and bring the summary of your experiences to your appointment. This gives your doctor a clear, concise starting point for your conversation, ensuring you cover the most important points during your visit.
Disclaimer: This website provides a preliminary self-assessment tool for schizophrenia based on the Prodromal Questionnaire. It is not a diagnostic tool. The results are for informational purposes only and cannot replace a professional evaluation by a qualified healthcare provider. If you are concerned about your mental health, please consult a psychiatrist, psychologist, or other mental health professional.
Frequently Asked Questions About Bipolar Disorder & Schizophrenia Tests
How do I tell if I'm schizophrenic or bipolar?
While you can learn about the key differences, only a qualified healthcare professional can make an accurate diagnosis. Bipolar disorder is defined by distinct mood episodes (mania and depression), whereas schizophrenia is primarily a thought disorder with persistent psychosis. A helpful first step can be to document your symptoms, and a confidential online test can help you organize these observations before speaking with a doctor.
What kinds of tests confirm schizophrenia or bipolar disorder?
There is no single blood test or brain scan that can definitively confirm either condition. A diagnosis is made through a comprehensive clinical evaluation, which includes a detailed interview about your symptoms, personal and family medical history, and sometimes a physical exam to rule out other causes. Tools like an online schizophrenia test are screeners, not diagnostic tests.
Can a "mild" form of schizophrenia be mistaken for bipolar symptoms?
Yes, the early or "prodromal" phase of schizophrenia can be challenging to distinguish. Symptoms like social withdrawal, mood swings, and unusual thoughts can overlap with bipolar disorder. This is why a thorough differential diagnosis in mental health by a professional is so critical to ensure the right treatment path is chosen from the start.
Can you fully recover from schizophrenia or bipolar disorder?
While both are considered chronic conditions, recovery is possible. For many, recovery means learning to manage symptoms effectively to live a full and meaningful life. With consistent, appropriate treatment—including medication, therapy, and strong support systems—many individuals with these conditions achieve significant long-term stability and well-being.
Why is an accurate diagnosis so important for effective treatment?
An accurate diagnosis is the cornerstone of effective treatment because bipolar disorder and schizophrenia respond to different types of medication and therapeutic approaches. For example, mood stabilizers are central to treating bipolar disorder, while antipsychotics are the primary medication for schizophrenia. An incorrect diagnosis can lead to ineffective treatment, delaying recovery and potentially worsening symptoms.